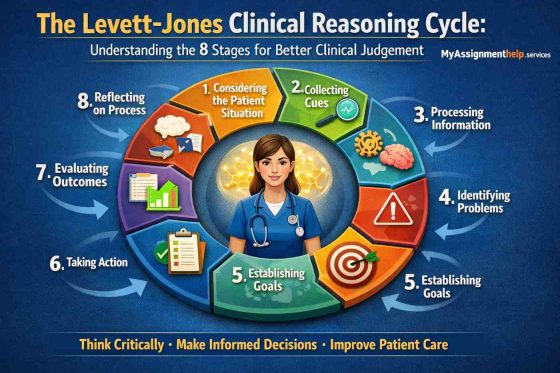
The Levett-Jones Clinical Reasoning Cycle: Understanding the 8 Stages for Better Clinical Judgement
The Levett-Jones Clinical Reasoning Cycle guides nursing students in clear thinking. It also guides in discovering patient issues more quickly. The 8 stages of this cycle are very confusing to many students. Each step is not complicated with easy guidance. This guide will make this stage very easy, simple, and readable for you. It presents the easy steps clearly, which you can follow in your study and case studies. This guide will make you score higher and have more confidence.
- If you want expert guidance for exams and assignments, you can connect with MyAssignmentHelp. Our platform has local expert help that is original and AI-free.
Introduction: The Blueprint for Australian Nursing Excellence
The Levett-Jones Clinical Reasoning Cycle is the most important thinking tool for a nursing student in Australia. This Cycle is a systematic model. It is used to collect and process information. This model also helps to make informed decisions. Australian nurses use this model in 8 stages. Most nursing programs at the University of Technology Sydney have this model. Monash University and the University of South Australia also teach this model as an important part. It also aligns with the NMBA Standards. It provides guidance for safe and professional nursing care in Australia. Some students feel stressed because of studying, jobs, and assignments. We have Assignment Help Australia to offer extra help for your better understanding.
This cycle is not just a study topic. It is the foundation of patient safety in Australian hospitals. Nurses apply it to the patient’s story to make a proper decision. This cycle helps them to understand what should be done. It results in improved outcomes. Once you master this cycle, you will feel more confident. You can easily complete your assessment and case studies, as well as clinical skills.
In the starting phase, you can feel this cycle is more difficult than it seems. The 8 stages are confusing for most Australian nursing students. Others struggle to relate cues, process information, or state the actual problem. The rest do not know how to formulate goals or reflect on their choices. This guide will explain the clinical reasoning cycle stages for you with line-by-line explanations. It will guide you in gaining a clear understanding of the model. You can think of a nurse in simple steps. You will know how to apply stages in actual practice and assessment.
What is the Levett-Jones Clinical Reasoning Cycle?
The Levett-Jones Clinical Reasoning Cycle is a model of thinking for nurses. Tracy Levett-Jones has developed this model. She structured it in such a way that it can help the nurses in making safe and clear decisions. Nowadays, this model is very common in Australian nursing schools. It is applicable in real hospital cases. In Australia, many people call it the gold standard.
This model does not match ADPIE. ADPIE is a simple list. You go from one step to another. It does not highlight the way nurses think. It fails to show the changing decisions of the nurses when the patient is changed. It is straight and fixed.
The model of Levett-Jones is a cycle. It is flexible. It is possible to go forward or back at any stage. You can think again. You can check cues again. You can adjust your actions. This brings reality to the model. It shows the work of nurses in a clinical context, which is more hectic. It also aligns with the NMBA Standards. This standard gives guidance on safe nursing care.
This cycle guides the students to realise the reason behind their decision. It helps you notice patterns. It helps you think deeper. It even helps you to prioritise patient safety. That is why this model is more popular in Australian universities. Hospitals choose this model over a simple checklist.
Clinical Reasoning vs. Clinical Judgement
These two words are similar; however, they are not the same. A high number of students confuses the two terms. Let’s clear your concept without confusion. They are not identical; however, they sound similar. These two collaborate, although both of them play different roles in nursing care.
Clinical reasoning is a process. It is the thinking process. You collect cues. You understand them and plan what to do. You align the situation of the patient with your knowledge. You also look at the presence of something that seems to be dangerous. Clinical thinking is slow and needs to be careful. It is a cycle that continues to repeat with patients’ change.
The last option is clinical judgement. It is a choice that you make after all the thinking. It is the place where you decide on which action is suitable. It is up to you to decide which problem is the most important. You plan what to do next. You are the one who decides whether the patient is improving or deteriorating.
In simple words:
Clinical reasoning = how you think.
Clinical judgement = what you decide.
The 8 Stages of the Clinical Reasoning Cycle (The Core)
The Levett-Jones Clinical Reasoning Cycle involves eight steps. It guides the nurses to make safe and clear decisions. You can easily feel confused about understanding these different stages. Let’s help you understand these stages without making it difficult. Understanding these stages is easy when you break them into simple points. The stages allow you to think, make a strategy, and take action. It helps you to reflect like an actual nurse in Australian hospital environments. Below, the stages are explained simply.
Before the stages, here is a short comparison for clarity:
Levett-Jones vs. ADPIE (Short Comparison)
- ADPIE is a straight checklist. You move step by step. You cannot go back easily.
- Levett-Jones is a cycle. You can move forward or go back anytime.
- ADPIE tells you what to do.
- Levett-Jones explains how you think.
- ADPIE works on basic tasks.
- Levett-Jones is better for real, complex patient care in Australia.
2.1 Stage 1: Consider the Patient
This step is used to know the beginning point of care. You develop a fast and clear picture of the situation of the patient.
What you focus on:
- Why the patient is here
- What the patient looks like
- How the patient sounds
- Their main concern
- First signs of distress
Example: A 65-year-old female patient says, I am unable to breathe properly. She seems pale, anxious and tired. Her breathing is fast.
This is the level of awareness. You are ready to move on to the next step.
2.2 Stage 2: Collect Cues / Information
In this case, you collect all the information about the patient. This involves facts, indicators, symptoms and accounts.
Focus on the difference:
- Subjective data = the statement of the patient
- Objective data = what you see, measure, or read
Subjective examples:
- “I feel dizzy.”
- “My pain is sharp.”
- “I cannot breathe well.”
Objective examples:
- Vital signs
- Lab test reports
- Wound appearance
- Oxygen levels
- Nurse handover notes
- Medication charts
Key points:
- Read the notes carefully.
- Listen to the patient.
- Observe everything.
- Collect facts, not guesses.
2.3 Stage 3: Process Information
This is the most important and key thinking phase. You transform unprocessed data into understanding and information.
You use key cognitive skills:
Pattern Recognition
You notice common patterns that point to a likely issue.
Example: Low O₂ + fast breathing + wheeze = airway or lung problem.
The Difference between Relevant and Irrelevant:This is critical to nursing learners. It is up to you to decide what is right at this moment.
Relevant:
- Breathing pattern
- SpO₂
- Wheeze
Not relevant (for now):
- Past knee surgery
- Old social history
- Minor unrelated complaints
Predicting Risk
You consider what is going to follow:
- Is this to turn out to be respiratory failure?
- Is urgent care needed for the patient?
- Should I escalate early?
Linking Cues Together
You relate the information to gain a clear picture of the patient’s situation.
This phase takes you out of the data gathering and into the problem understanding.
Example: Shallow breathing, less oxygen, and chest tightness – pattern highlights a respiratory problem.
2.4 Stage 4: Identify Problems / Issues
Now, name the primary problem. Your thinking and the cues guide you to make a decision. It sets the highest priority.
Key points:
- Identify the urgent issue.
- First, decide what will be harmful to the patient.
- Select the issue that should get fast action.
Examples:
- Acute pain after surgery
- Shortness of breath
- Risk of infection
- Low blood pressure
- Dehydration
It is a critical step in completing assessments. Students often face failure to prioritise correctly. It is likely to cost you some marks.
2.5 Stage 5: Establish Goals
You now create the objectives for the patient. The following objectives will help you create your care plan.
Use the SMART method:
- Specific
- Measurable
- Achievable
- Relevant
- Time-bound
Examples:
- The pain of a patient will lessen to 3/10 in an hour.
- In 30 minutes, the oxygen level will be 95%.
- Fluid intake is to become 1500 ml in 24 hours.
Key points:
- Goals must match the problem.
- Goals must be realistic.
- Goals must have a clear time limit.
2.6 Stage 6: Take Action
This is the place where the plan is executed. You select the most appropriate evidence-based interventions.
Examples of actions:
- Give prescribed medicine.
- Adjust oxygen flow.
- Reposition the patient.
- Clean and dress a wound.
- Encourage fluid intake.
- Call the doctor if needed.
- Follow hospital policies.
Key points:
- Act safely.
- Follow guidelines.
- Use critical thinking.
- Document your actions.
2.7 Stage 7: Evaluate Outcomes
You now look into whether the action was effective or not. You look at the patient again.
Key points:
- Did the patient improve?
- Did the signs change?
- Did the pain reduce?
- Are vital signs better?
- Is the goal met?
- Do you need to change the plan?
Examples:
- Pain lessened from 8/10 to 3/10
- Oxygen improved from 89% to 96%
- The patient can move with a lesser amount of effort
This step guides you in deciding whether the care was successful or not.
2.8 Stage 8: Reflect on Process
The last stage of the Clinical Reasoning Cycle is reflection. It is the place where you reflect on your actions and consider what you learnt. Reflection will make you a better student nurse. It will prepare you to create improved clinical judgment in the future.
What you reflect on:
- What went well
- What was difficult
- What would you change next time
- How you felt
- How you handled stress
- How you communicated
- What you learned about yourself as a nurse
Examples:
- I acted quickly when I saw the oxygen drop.
- Next time, I will have to gather cues more quickly.
- I remained calm and described care in a problem-solving manner.
Comparison: Levett-Jones Reflection vs. Gibbs Reflective Cycle
There are many students who confuse these two models. Knowing the difference helps to have a clear idea.
1. Purpose
- Levett-Jones reflection is related to the extent to which you went through the steps of clinical reasoning.
- Gibbs Reflective Cycle guides you to look more into how you feel. It helps you in action and how you learn.
2. Structure
- There is one reflection stage at the end of the cycle in Levett-Jones.
- Gibbs employs 6 phases: Description, Feelings, Evaluation, Analysis, Conclusion, and Action Plan.
3. Use in assessments
- Levett-Jones is used when reflecting on clinical decisions.
- Gibbs is applied when you make reflections on self-development, emotions and practice.
4. Depth
- Levett-Jones reflection is brief and prioritises decision-making.
- Gibbs is more timely and emotive.
In case you need to reflect on an assignment, you can go through the Gibbs Reflective Cycle. It provides a clearer guide to writing reflection paragraphs.
Summary Table: The 8 Stages at a Glance
This table provides a brief overview of all eight stages of the Levett-Jones Clinical Reasoning Cycle. It is created for students who want a quick revision before writing a case study. The design of this cycle also helps in giving an exam or preparing for a placement. To make it simple, the example of the same patient is used in every stage, the patient’s shortness of breath. This process will keep it simple for you to understand. You will see how the cycle moves from one stage to the next in a real clinical situation.
| Stage Name | Primary Action | Quick Example (Shortness of Breath Patient) |
| Stage 1: Consider the Patient | Understand the situation and main concern | Patient informed, I am unable to breathe properly. She seems pale, anxious and tired. Her breathing is fast. |
| Stage 2: Collect Cues / Information | Collecting subjective and objective information | Says chest feels tight (subjective). O₂ 88%, RR 30, wheeze present (objective) |
| Stage 3: Process Information | Use pattern identification and makes sure what matters | Low oxygen + fast breathing + wheeze → likely airway or lung problem |
| Stage 4: Identify Problems / Issues | Choose the top priority problem | Key issue: fast breathing and low oxygen saturation |
| Stage 5: Establish Goals | Set SMART goals for the patient | Increase O₂ to 95% within 30 minutes; reduce RR to 20/min |
| Stage 6: Take Action | Taking the nursing actions | Apply oxygen, sit upright, monitor vitals, call doctor if patient condition gets worse |
| Stage 7: Evaluate Outcomes | Check if actions was effective | O₂ rises to 95%, breathing improves, patient gets clam |
| Stage 8: Reflect on Process | Reflect on what you learned | I acted quickly when I saw the oxygen drop. Next time I will have to gather cues more quickly. |
Stage 1 guides in creating the initial image of the patient.
Stage 2 guides in gathering together all the important information. This information is subjective and objective, which is the basis of thinking.
Stage 3 is the most important level of thinking. Here, you apply pattern recognition and decide the relevant and irrelevant cues.
Stage 4 helps in prioritising the problem that is significant to safe care.
Stage 5 involves you setting SMART goals to have your care plan organised.
Stage 6 is the action place where you act. It may be oxygen, medication, repositioning, or calling for help.
Stage 7 monitors the success of your plan. Whether the action worked or you must change it.
Stage 8 develops your learning and growing professionally.
The table is applicable in assignments for OSCE preparation. It is also useful for lab work in clinical environments and rapid revision. In case you wish, I can also make a downloadable copy in PDF format for the students.
Practical Application: Clinical Reasoning Cycle Case Study (Australia)
This clinical reasoning cycle case study shows how a nurse applies each stage during a real shift in an Australian hospital.
Scenario:
A post-operative patient: Day 1 after abdominal surgery, suddenly develops tachycardia (HR 132), pale skin, and low blood pressure. The nurse begins the cycle.
The nurse thinks: “Something is wrong. He did not look like this an hour ago.” She considers the patient’s history and notes the sudden change in his condition.
Next, she collects cues. She gathers subjective cues: “I feel light-headed” and objective cues HR 132, BP 88/50, cool skin. “These numbers are not normal,” she thinks while checking the chart.
She processes the information. She recognises a pattern: fast heart rate + hypotension + pale skin. “Could this be internal bleeding? Is this a post-op complication?” She separates relevant cues and predicts risk.
She identifies the priority issue: “Possible haemorrhage.”
Her goal becomes clear: “Stabilise him and prevent deterioration.”
She takes action immediately. She raises a MET call, lays the patient flat, increases IV fluids, and uses the ISBAR method to hand over:
“I: Post-op patient. S: Sudden tachycardia and hypotension…”
Then she evaluates outcomes. The MET team arrives, and vital signs slowly improve.
Finally, she reflects: “I recognised the signs early. Next time, I will check post-op vitals more often.”
This case shows how the cycle improves safety. Nursing care study help is essential for rapid decision-making in Australian clinical settings.
Real-World Nursing Case Study Examples (Australia)
These nursing case studies from Australia show how different patient problems appear across real Australian healthcare settings. All short scenarios are a reflection of the typical issues students face. They face issues in placements, examinations, and clinical tests.
1. Surgical Case (Post-Operations Complication), Private Hospital, in a city
This is a 54-year-old male who came to one of the non-government hospitals located in Sydney. He felt sharp pain in the abdomen after he had bowel surgery. His heart beat increases up to 125 Bp. his stomach becomes firm. The nurse believes this may be early sepsis or internal bleeding. She proceeds to check the patient’s vitals and calls the surgical registrar. She prepares fluids and puts the patient on nil by mouth. Immediate response lowers deterioration. This is a typical post-Op case that is common at large Australian hospitals.
2. Community / Aged Care Scenario (Polypharmacy Regional Aged Care Facility)
An 82-year-old woman with a regional Victorian aged care home struggles with confusion and continuous falls. She is using eight medications. The registered nurse questions, “Is that polypharmacy? She goes through the drug history, measures the pressure, and finds that the resident is light-headed when she stands. She calls the GP and requests a medication assessment and changes the care plan. The case shows the general problems of aged care in Australia, particularly in the regions and rural settings.
3. Mental Health Scenario (Rural Remote Clinic – Suicide Risk Assessment)
The case involves a 22-year-old male reporting to the rural clinic in Western Australia with low mood and poor sleep. He has lost his job recently. He mutters, sometimes it seems to me it is too hard to go on. The nurse undergoes a suicide risk assessment, maintains safety and calls the mental health crisis team. She keeps him safe until the arrival of help. This situation highlights how important mental health nurses are in isolated societies.
These nursing research topic examples show how broad skills are needed for nurses in various settings of care.
Assignment Success: How to Get a High Distinction (HD)
To get a high distinction score, you need to highlight good reasoning and proper structure. You also need to show well-made connections between cues and decisions. Students frequently lose points by being too descriptive and not analysing. They also put the misplaced focus on the priority problem or confusion of personal and objective facts. Others also overlook the Reflect stage. You can get guided support, or you can request Nursing Assignment Help.
Use the right style:
Stages 1-7: third person (The nurse noticed.)
Stage 8: first-person stage (I realised… )
Give more words on Stages 2, 3 and 4, which display deep thinking. Stages 1, 5, 6, 7 and 8 do not have to be long but should be clear. These steps will assist you in providing a good, detailed response, which is well structured and scored. You can also use UTS referencing tools.
Common Mistakes Students Make
- Writing too much description and not enough analysis
- Forgetting to explain why a cue is important
- Ignoring the “Reflect” stage
- Choosing the wrong priority problem
- Not using subjective and objective data correctly
- Weak justification for goals and actions
- Poor alignment with Australian clinical guidelines
- No link between cues and the final judgement
Stage 8 (Reflect): Write in first-person use
- Example: “I realised that…”
- Example: “I learned that…”
Reflective essay writing is about thinking about your past actions and writing what you felt. You need to reflect on your good skills, actions and what needs improvement.
Free Download: Clinical Reasoning Cycle Case Study Template
Here is a simple clinical reasoning cycle case study template that students can copy and paste into their Word document. It follows the Levett-Jones structure, uses clear headings, and keeps the layout clean. This template helps you plan your assignment, write in order, and stay aligned with Australian nursing expectations.
Use it for case studies, OSCE notes, assessment drafts, or quick practice before exams.
Clinical Reasoning Cycle Case Study Template (Copy & Paste)
1. Consider the Patient
Write the patient’s story. Include age, setting, main concern, and first signs.
2. Collect Cues / Information
Add subjective data (what the patient says) and objective data (what you observe or measure). Include vitals, charts, handover notes, and health history.
3. Process Information
Explain what the cues mean. Discuss patterns, red flags, and relevant vs irrelevant information.
4. Identify Problems / Issues
State the priority problem. Link it clearly to the cues.
5. Establish Goals
Write SMART goals. Make them specific, measurable, achievable, relevant, and time-bound.
6. Take Action
List the nursing actions you will take. Use evidence-based practice and Australian guidelines.
7. Evaluate Outcomes
Explain whether the actions worked. Show changes in vitals, symptoms, and patient comfort.
8. Reflect on Process
Write what you learned. Use first person (“I realised…”). Mention how you will improve next time.
This template makes your assignment faster, clearer, and more structured.
Semantic Comparison: Levett-Jones vs. Tanner vs. ADPIE
Australian nursing programs often choose the Levett-Jones Clinical Reasoning Cycle because it teaches students how to think, not just what to do. It focuses on the entire reasoning process, from collecting cues to reflection, which makes it ideal for case studies, OSCEs, and undergraduate assessments.
Levett-Jones vs. Tanner’s Model of Clinical Judgement
Tanner’s model focuses strongly on two steps: Noticing and interpreting. It explains how nurses understand patient cues and make sense of the situation. This makes Tanner very useful for analysing thinking patterns.
However, Tanner’s model is less structured when it comes to action. It tells you how nurses think, but does not give a clear path for:
- Setting goals
- Acting on decisions
- Evaluating outcomes
- Reflecting using a cycle
In contrast, Levett-Jones provides a full, step-by-step action pathway. After thinking, the model shows exactly what the nurse should do next. This is why universities prefer it for assignments—it matches the real flow of clinical care in Australian hospitals.
Levett-Jones vs. ADPIE
ADPIE is simple and linear. You move from one step to the next. It is easy but limited. It does not show how nurses rethink or loop back when a patient’s condition changes.
The Levett-Jones cycle, however, is recursive. Students can move forward or return to earlier stages. This mirrors real Australian clinical practice, where patient conditions shift rapidly.
In summary:
Tanner improves thinking.
ADPIE improves organisation.
Levett-Jones improves clinical reasoning and action, making it the preferred model for nursing education in Australia.
FAQ Section
1. How many stages are in the clinical reasoning cycle?
There are eight stages in the Clinical Reasoning Cycle. These stages guide nurses through understanding the patient, collecting cues, thinking about the information, identifying problems, setting goals, taking action, checking outcomes, and reflecting on the process.
2. Why is the Levett-Jones model used in Australia?
It is used because it teaches nurses how to think, not just what to do. The model matches real Australian clinical practice, supports NMBA standards, and helps students make safe, evidence-based decisions. It is also widely used in nursing assessments and case study tasks.
3. What is the difference between a cue and an inference?
A cue is a fact, such as “BP is 90/60”. An inference is what you conclude from that fact, such as “the patient is hypotensive.” Cues are observations. Inferences are interpretations. Nurses must separate the two to avoid errors in clinical judgement.